

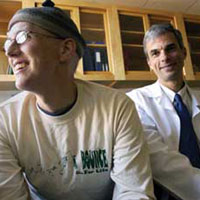
In the aftermath of Hurricane Katrina, Tyler Curiel (right), the chief of hematology and medical oncology at Tulane University School of Medicine, worked tirelessly both to care for his patients at Charity Hospital and to protect irreplaceable research samples at the University's Health Sciences Center. Top among his concerns was saving a rare line of cancer cells that his former protégé Andy Martin (left) had cultured from his own tumor before he died in November 2004. |
On January 16, 2006, Tyler Curiel answered selected viewer questions about his research and his experiences during Katrina and the storm's aftermath. Please note we are no longer accepting questions, but see our links and books section for additional information. Below, read answers to a wide range of questions viewers have e-mailed. Q: After all you have gone through because of Katrina, have you thought about relocating your work outside of New Orleans? Are you worried that another hurricane could cause an even more devastating loss of research in the future? A: Dear Stacy, Yes, I remain very concerned. We are looking now at placement of emergency generators so that they are above the maximal tidal surge height (about 22 feet), and placement of helipads to lift in fuel and supplies as needed. We are also evaluating the communications and other systems that failed post-Katrina. Of course, we await the final plan on rebuilding our levee system, which is the single most important factor in working safely in this environment. Provided that safety can be ensured as best as can be expected in this area, and if the post-Katrina plans meet my expectations and can be effected in a timely manner, I will keep my operation at Tulane. Q: Are you rebuilding your lab in some different way to anticipate future hurricanes? Is Tulane taking any special steps to prepare for future storms? A: Dear Jason, Please see my response above. Also, Tulane University is evaluating its hurricane preparedness plans and infrastructure. No final decisions have been made on the entirety of the plan, but I am sure that you can imagine how much attention it is getting. We are working very hard to correct deficiencies. Q: When do you expect your lab to be back up and running? Have any of your lab members decided not to move back to New Orleans? A: Dear Anonymous, I currently have functional labs operating at the Tulane Primate Center, in Baton Rouge, at the University of Colorado, and at other locations. Our clinical trials are continuing to enroll patients and meet their goals. Labs in Tulane Medical School remain largely unusable at present (January 16, 2006) but should be functional by the end of February or early March. Nonetheless, we are currently able to continue critical lab functions by using temporary space in the adjoining J. Bennett Johnston Building, and at the off-site locations just mentioned. One member of our clinical faculty decided to move to San Francisco, two post-doctoral students elected to move to other locations, and one administrator was let go because of a required downsizing. All remaining physicians, scientists, technicians, aides, students, and staff are already back, or will come back when appropriate facilities are available. I am extremely fortunate in this regard. Q: You are clearly passionate about your work, and your devotion to your research and students is an inspiration. When and how did you decide to become a cancer researcher? A: Dear Lisa, I always knew that I wanted to be a scientist. Since the fourth grade I was building model rockets, collecting fossils, and going to science camps. I initially wanted to be a rocket scientist (no fooling), but NASA reduced its space program after the Apollo program finished, so I looked elsewhere and went to medical school knowing that I would do some kind of medical research. In medical school I was trying to decide between infectious diseases and cancer. I eventually chose infectious diseases research because I wanted to work for David Durack, the chief of that section. Taking a year to do research with him was one of the best career decisions I ever made. I came back to cancer about 10 years later as I was seeing a large number of cancer cases in our AIDS patients. Eventually I decided that research in cancer immunology was even more of a mess than AIDS immunology and decided to take on the challenge. Q: As a graduate student who was working in a research hospital in Manhattan on September 11, 2001, my heart went out to those scientists and doctors who faced great adversity in New Orleans during Hurricane Katrina. Your story and your dedication to keeping the work and memory of your student Andy alive really moved me. It was good to see such personal dedication to the life of one person as well as seeing that not everything was lost in the face of Katrina. A: Dear Jason, Thanks for the kind words. There were many individuals working long and hard under dire circumstances to treat patients, save lives, and rescue the research. Q: What do you hope to accomplish with your research? What will this research provide to the medical community? A: Dear Marcus, Immune therapy for cancer has the potential to eradicate all cancer, just as it can eradicate all influenza virus in an infected person. We have to learn how to harness the potential of immune-based therapy in cancer. Our lab focuses on determining why cancers are not immunologically rejected as foreign, just as a mismatched kidney transplant would be rejected. If we succeed, cancer treatments may become more successful and more specific (meaning with fewer side effects). Unfortunately, we are still a long way from that goal, although we have made tremendous strides as a scientific community in the past decade. Q: Would a typical GP know of Andy Martin's cancer [SNUC]? My 17-year-old daughter is having problems with nosebleeds, and a recent exam revealed only a small, unidentified bump in her nose. Thank you! A: Dear Steve, SNUC is very rare and can be difficult to diagnose. A typical GP likely will have no experience with it and probably has not even heard of it. Fortunately, most GPs know when to refer to a specialist as necessary for further investigations. Even more fortunately, most nosebleeds are not caused by SNUC (or any type of cancer for that matter). Q: We were amazed not only by your tireless effort to save your research materials but also by your ultramarathon running. How do you find time to do all that running and your lab work too? Do you think running helps you in your research work? Do you think your experience in marathons helped you through Katrina? A: Dear Nancy and David, Running keeps me relaxed and focused. I get many of my best research ideas on a long run, when the phone can't ring, my pager can't go off, and no one will interrupt. I spend far fewer hours each year training to run ultramarathons than the typical American spends watching TV. Since I don't watch TV (no offense to NOVA!), that frees up lots of additional time. Being prepared for ultramarathons unquestionably was a big advantage for me. I was able to work fast and hard for long stretches, go up and down innumerable stairs on errands, and endure food and water shortages better than most. I actually wore my 100-mile racing clothes and fanny pack (which included a headlamp to see in the dark) the entire time we were stranded after Katrina. I recounted how my ultramarathon training helped me during Katrina's aftermath in the November 2005 issue of Ultrarunning magazine. Q: Did many of your colleagues at Tulane lose their research? It's tragic to think of all the work that might have been destroyed by the flood. A: Dear Sally, Unfortunately, much precious research was lost forever, the biggest example being the Bogalusa Heart Study. This study had a frozen repository of blood spanning over 40 years that melted and was ruined. Other researchers also suffered big losses. Still, Tulane estimates that 85 percent of the critical research was salvaged, which is a tremendous achievement. The millions of dollars and thousands of person-hours lost are still being tallied. Q: I saw your story on NOVA tonight. Please consider the very prudent practice of storing half of your critical and irreplaceable cell lines at an offsite storage facility/repository. I own a facility and would be happy to offer our services at a greatly reduced storage rate. A: Dear Michael, Thank you for this suggestion, which is under consideration. Q: I have two questions, if you don't mind. The first question is concerning the research that was recovered. What percentage of the research that was brought back is currently being used in your daily search for clues to the cure and /or treatment of small cell cancers? The second question deals with the rescue mission itself. In your opinion, was the Hawker 600 you flew down in smoother than the Gulfstream that picked you and the staff up after the hurricane, or were the sandwiches just better? A: Hi Brian, Readers should know that Mr. Perryman, through his company Phazar, along with Pete DeLisa of Trident Aviation, donated the use of their airplanes to us on two separate occasions—first to evacuate all 19 staff remaining in Charity Hospital one week after Katrina, and second to let me go back with a crew and supplies to effect the research rescue the following week. Hats off, gentlemen! Without generous and selfless acts such as yours, much additional work would have perished. I convey my personal thanks and gratitude on behalf of Tulane. We don't specifically work on small cell cancers, but the work we do should be applicable to it. Regarding the airplanes, I would like a Gulfstream for my next birthday if it's not too much trouble. The Hawker was smoother, but I still enjoyed the food in the Gulfstream better. Perhaps it was because it was the first good meal that I had after being evacuated. Q: I'm a member of the flight crew, EAGLE 1 Police Rescue helicopter from Connecticut, who flew Dr. Curiel to Tulane to get the research that was almost lost due to the hurricane. I have photos of that mission where we had to land on the roof of the parking garage. If the photos would be helpful to you, let me know. A: Hi Paul, Thank you so much for the professional and efficient manner in which you and the entire flight crew managed operations. We always felt like we were in great hands, and I appreciate your commitment. I especially enjoyed your comment that if I pointed out the wrong landing spot on the top of the parking deck as we searched visually from the air, and the chopper fell through to the basement, that "it would really ruin our day." Yes, I would greatly appreciate the photos. Q: I just want to thank you for taking part in the wonderful NOVA scienceNow segment. The story about the cell line from the medical student Andy Martin brought tears to my wife's and my eyes. Our best wishes go to you and your colleagues at Tulane Medical School as well as to Andy Martin's family. Can you tell us about any research progress that has been made using Andy Martin's cells? A: Dear Michael, Thanks for the kind words, which I accept on behalf of the entire research team. Progress has been slow but steady. We are now shipping some of our Andy Martin SNUC cells to the National Cancer Institute for genetic testing on gene chips to help determine what makes them so aggressive. Q: I am a former resident of New Orleans, and to say that my wife and sons miss the city is an understatement. To learn of your extraordinary efforts on behalf of humankind is inspiring. To know that it comes from my birthplace makes a native son proud. New Orleans is special for much more than the food and music ... it is Tulane and the other gems such as Xavier and St. Augustine and Jesuit High schools that lend texture to the fabric of a great city. LONG LIVE NEW ORLEANS!!! America and the world will not be the same without the Crescent City. A: Dear Joseph, Amen. The work and the rebuilding go on. Q: I'm a stage IV ovarian cancer survivor dx 11/04. I had three neoadjuvant carbo/taxol, then debulking and three more carbo/ taxol. I now have three more of 12 taxol consolidation tx to go and have no evidence of disease. I hope I never recur, but I had followed with interest your "Treg" research and trial before Katrina. What were you able to salvage and where does this research stand at this point? Thank you!! A: Dear Pat, Fortunately we salvaged all our ovarian cancer and Treg work. The two clinical trials remain active, and we are treating patients. I am discussing a combined Ontak/vaccine trial with the National Cancer Institute and another trial with a biotechnology company. Both are for ovarian cancer. Good luck with your treatments. Q: Dr. Curiel, I was very excited and shocked to see you on NOVA last night. I am a 50-year-old male who was just diagnosed with SNUC, on December 22, 2005. It all started about two months ago when I was having problems with my right ear not draining. I went to the doctor, and she gave me antibiotics for the ear. It did not seem to help me any, and then out of the blue my neck started to swell. Finally after many more tests my ENT decided to do exploratory surgery. The tissue from my sinus was sent to the Mayo clinic. The result was SNUC. My doctors want nothing to do with the treatment, so they are going to send me to MD Anderson in Houston, Texas. I have been doing a lot of research and finding out just how rare and deadly this disease is. However, I have found people who have seemed to survive SNUC, but for how long I do not know. I would like to know if any more information has been acquired from your research or any other physicians you know. Thank you to you and to all the others like you for putting in all the sleepless nights trying to make people like me live longer. A: Dear Lynn, I am sorry to hear about your diagnosis. MD Anderson is one of the best places for SNUC treatment in the world. We have discussed our work with them, and we are looking to collaborate in the future. I wish you well with your treatments. |
||||||||||
|
|
|||||||||||
|
© | Created January 2006 |
|||||||||||