
|
 |
|
O. H. Frazier Part 2 | Back to Part 1 NOVA: What are the advantages of continuous rather than pulsatile (pulse-like) flow? Frazier: With continuous flow, there isn't a pulse. Without a pulse, it is not necessary to have volume compensation for the heart. If volume compensation isn't needed, then we don't have to penetrate the skin. If we don't have to penetrate the skin, then we can do away with what I think is the most important problem with long-term devices being used now—infection. So, continuous flow has many advantages, although it wasn't widely considered until recently because we didn't know whether patients could live without a pulse. Maybe complications would result from pulseless flow. Maybe nature intended for us to have a pulse. How do you feed the pump that pumps the blood (and nutrients) to the rest of the body? The only way to do that is to give the heart a rest. So, we have a pulse to allow the heart to get its rest and renewed energy. It's a remarkable organ in that regard. NOVA: Do you think the AbioCor total artificial heart [which is slated to begin human trials in the year 2000] is ready for use in human patients? Frazier: We're very anxious to use this technology because we will be able to help patients who aren't being helped now. I think we've validated this concept biologically more than adequately. We have studied more than 100 animals with the AbioCor heart, some for more than 100 days, and the pump has worked very well. If it lasts that long in animals, it will work in humans. Reliability testing and further wear testing are ongoing. NOVA: What are the specific advantages of the AbioCor heart?
The AbioCor artificial heart is small, and it was designed for the human heart. The first artificial hearts were designed more for the calf, and the first patients who received those devices were large people. Barney Clark, for instance, was a huge man. He weighed more than 300 pounds, and he was well over 6'4" tall. But the AbioCor pump is designed for the average-sized adult. It's still too big for small adults, but it will fit in most of the U.S. adult population. Another advantage is that the AbioCor pumps alternately right to left. So it doesn't pump both to the lungs and the body at the same time, like the normal heart, but it pumps side to side. This is an important advantage, because the bulk of the volume compensation that a pulsatile pump needs can be adjusted by using alternating ventricles. So when the left side is pumping, the right side is a volume chamber, and vice versa. NOVA: Why is that important? Frazier: Well, the right heart and the left heart don't pump the same amount of blood; the left heart pumps more. So there has to be some way of compensating for that variance between the two sides of the heart and the amount of blood pumped. This has been done in a very ingenious way by the engineers who developed the AbioCor heart—a really outstanding engineering accomplishment. They designed a small compensation chamber, which acts in a way to allow the right side of the heart to sense whether it needs to pump more blood or less blood. It automatically adjusts internally according to changes within this little chamber.
NOVA: Which patients do you think the AbioCor will benefit most? Frazier: The bulk of patients who die within a few days after a heart attack or after open-heart surgery could benefit from these pumps, because they need both ventricles. Artificial hearts are like transplants except they can't be rejected, and they can also be produced in unlimited quantities. NOVA: And the AbioCor will be totally enclosed within the body? Frazier: Yes. The technology to transmit energy across the skin—that is, without going through the skin—has been available for years. Remember the high school experiment in which you lit an electrical bulb by bringing an electrical field close to the bulb? It's the same principle. A small coil inside the body can be supplied with energy from a small coil on the outside of the body during day-to-day activities. The pump will also have a small internal battery that will supply energy for short periods of time when power needs to be completely internal, like when a patient is taking a shower. And it's totally quiet. Because of that, I think patients will be able to go back to work easily. Patients with these hearts will look like anyone else—with no tubes or wires to be seen. These patients will be able to work and live in much the same way as a normal person does. NOVA: Will we still need LVADs and other heart-assist devices?
When we first started using the HeartMate in 1986, we used it in very few patients. Last year, more than 500 patients in the United States who would have died had this pump implanted. But the need is still much greater than that, because the number of patients dying prematurely of heart disease is far in excess of what we should accept. I think that all of the very different technologies we have discussed will play a big role in the treatment of heart disease. To have all of these varying technologies available off the shelf is our goal. I'm not sure if it will take two years or 20 years, but I think it will be achieved. Photos: (1,2) NOVA/WGBH; (3) WGBH; (4) courtesy of Richard Wampler; (5,7,8) Texas Heart Institute. Map of the Human Heart | Amazing Heart Facts The Artificial Human | Pioneering Surgeon | Operation: Heart Transplant Resources | Transcript | Site Map | Electric Heart Home Editor's Picks | Previous Sites | Join Us/E-mail | TV/Web Schedule About NOVA | Teachers | Site Map | Shop | Jobs | Search | To print PBS Online | NOVA Online | WGBH © | Updated November 2000 |
 The Jarvik-2000 is gettIng close to human trials.
The Jarvik-2000 is gettIng close to human trials.
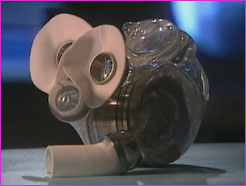 Beginning human trials soon, the AbioCor total
artificial heart will be entirely enclosed within the
chest.
Beginning human trials soon, the AbioCor total
artificial heart will be entirely enclosed within the
chest.
 Frazier believes that the new AbioCor heart will most
benefit patients who would otherwise die within a few
days after a heart attack or open-heart surgery.
Frazier believes that the new AbioCor heart will most
benefit patients who would otherwise die within a few
days after a heart attack or open-heart surgery.
 The HeartMate LVAD has been one of the more
successful of the left ventricular assist devices.
The HeartMate LVAD has been one of the more
successful of the left ventricular assist devices.